Abstract
Homeopathy has established its supremacy in the control of infectious viral diseases. The widespread acclaim in this regard is now supported by this study. The study was conducted in the Chikungunya fever hit areas of Kerala. The genus epidemicus was selected after detailed analysis of the first cases of Chikungunya. This preventive medicine was widely distributed in the disease prevalent areas. A survey was conducted for the evaluation of prophylactic efficacy. The study showed a very high significant effect of Homeopathic medicine in the prevention of Chikungunya fever.
Keywords
Homeopathy, Prophylaxis, Genus Epidemicus, Chikungunya fever.
Introduction
Homeopathic prophylaxis had its beginnings with the Father of Homeopathy, Dr Samuel Hahnemann (1755 – 1842). During a 1799 scarlet fever outbreak in Germany, Dr Hahnemann observed that three children in a family contracted the disease, but the fourth remained unaffected. The fourth had been treated with homeopathic Belladonna for an unrelated joint problem. Dr Hahnemann reasoned that perhaps the dose of Belladonna had protected the child from scarlet fever as well as treated the joint affliction. Soon afterward, he was able to test his theory when, in another of his patient’s families, three children in a family of eight contracted scarlet fever. Hahnemann administered homeopathic Belladonna to the remaining un-afflicted five, and all five remained symptom free. Hahnemann continued using Belladonna during this epidemic, and soon conventional physicians took note and began using the same protocol. Of 10 allopathic physicians who were reporting their results with Belladonna, 1,646 children were prophylactically treated and then exposed to scarlet fever, but only 123 children (7.4%) developed symptoms (during the same time, disease from exposure ran as high as 90%). Hahnemann subsequently detailed his success and prophylactic recommendations in an 1801 booklet called Cure and Prevention of Scarlet Fever.
In Kerala, there has been periodic outbreaks of epidemics, viz. Japanese Encephalitis, Weil’s disease, Cholera, Chickenpox, Viral Conjunctivitis and Dengue fever. The latest turn was that of Chikungunya fever.
Chikungunya is a relatively rare form of viral fever caused by an alphavirus that is spread by mosquito bites from the Aedes aegypti mosquito, though recent research by the Pasteur Institute in Paris claims the virus has suffered a mutation that enables it to be transmitted by Aedes Albopictus (Tiger mosquito). The name is derived from the Makonde word meaning “that which bends up” in reference to the stooped posture developed as a result of the arthritic symptoms of the disease. The disease was first described by Marion Robinson and W.H.R. Lumsden in 1955, following an outbreak on the Makonde Plateau, along the border between Tanganyika and Mozambique, in 1952. Chikungunya is closely related to O’nyong’nyong virus.
Chikungunya is not considered to be fatal. However, in 2005-2006, 200 deaths have been associated with chikungunya on Réunion island and a widespread outbreak in Kerala.
The symptoms of Chikungunya (also called as Chicken Guinea) include fever which can reach 39°C, (102.2 °F) a petechial or maculopapular rash usually involving the limbs and trunk, and arthralgia or arthritis affecting multiple joints which can be debilitating. There may also be headache, conjunctival infection and slight photophobia. In the present epidemic in the state of Andhra Pradesh in India, high fever and crippling joint pain is the prevalent complaint. Fever typically lasts for two days and abruptly comes down, however joint pain, intense headache, insomnia and an extreme degree of prostration lasts for a variable period, usually for about 5 to 7 days.
Dermatological manifestations observed in a recent outbreak of Chikungunya fever in Southern India includes the following:
1. Maculopapular rash
2. Nasal blotchy erythema
3. Freckle-like pigmentation over centro-facial area
4. Flagellate pigmentation on face and extremities
5. Lichenoid eruption and hyperpigmentation in photodistributed areas
6. Multiple aphthous-like ulcers over scrotum, crural areas and axilla.
7. Lympoedema in acral distribution (bilateral /unilateral)
8. Multiple ecchymotic spots (Children)
9. Vesiculobullous lesions (infants)
10. Subungual haemorrhage
Aims & Objectives
1. To assess the efficacy of Homoeopathic medicine in the prevention of Chikungunya.
2. To determine the magnitude of incidence, clinical features, mortality , social & economic impact of the Chikungunya epidemic.
Materials & Methods
After detailed analysis of Chikungunya cases in Neyyattinkara & Vizhinjam, the Genus epidemicus was selected to be Eupatorium perfoliatum. The 200th centesimal potency of this medicine was given in 15 doses (3 doses daily for 5 consecutive days). The distribution was done through various agencies, NGOs, FRAT etc. The details of distribution were recorded for the feedback study. The survey form for feedback study was prepared in Malayalam (Annexure-2A & 2B). The efficacy survey was conducted in the period of 20th – 30th November 2006 in the epidemic hit areas of Vizhinjam, Valiathura, Pothencode, Manacaud & Kamaleswaram, were preventive medicines were also distributed.
Survey Details
The field survey team comprised of 36 students of III BHMS course headed by the survey supervisor, Dr Sheela A. S (Head of the Dept. of community Medicine). The survey data entry team comprised of 52 Post Graduate students in the various departments. (Annexure-3). The Computerised data entry team comprised of 5 Post Graduate students. (Annexure-4). The Data analysis was done by subject experts.
Results & Discussion
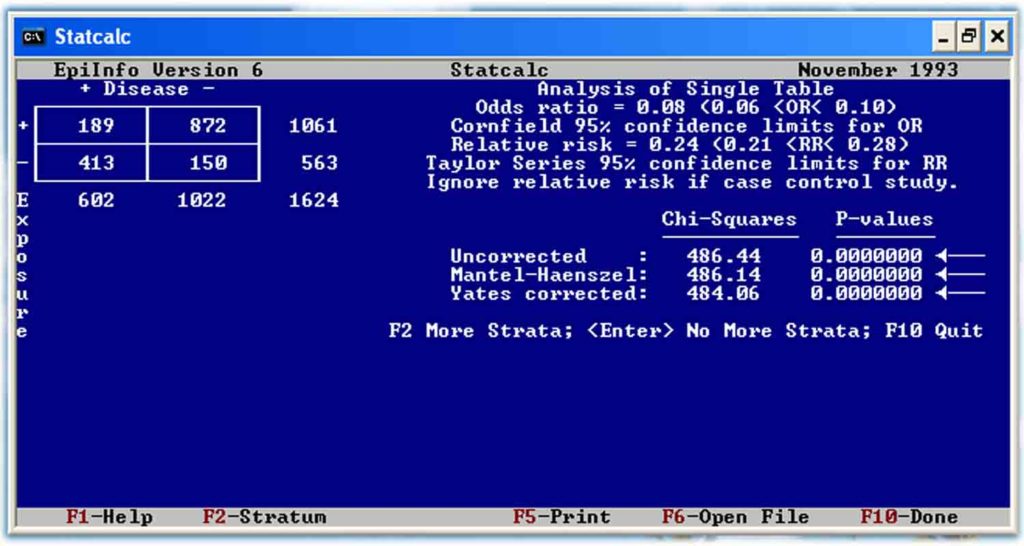
Total persons surveyed : 2000
Excluded cases : 376
Cases included : 1624
Treatment Group
Total no. of persons who have taken Homoeopathic Preventive Medicine : 1061
Total no. of persons who were affected with fever after the medicine : 189
No. of persons in which the preventive was effective : 872
% Efficacy : 82.19 %
Control Group
Total no. of persons who haven’t taken Homoeopathic Preventive Medicine : 563
Total no. of persons who were affected with fever : 413
No. of persons protected naturally ( ie, without medicine) : 150
% of cases protected naturally ( ie, without medicine) : 26.64 %
Statistical Analysis (see Annexure – 1)
Fever affected Fever not affected
Medicine given 189 872
Medicine not given 413 150
About the authors
Dr R. Rejikumar, Dr R. S. Dinesh etal