Abstract
Breast cancer (BC) is the most frequently diagnosed cancer in women throughout the world. The incidence and death rates have been increased over the last 30 years due to the change in risk factor profiles, better cancer registration, and cancer detection. The number of risk factors of breast cancer is significant and includes both modifiable factors and non-modifiable factors. Currently, about 80% of patients with breast cancer are people aged more than 50 years.
This review addresses the overview on the breast cancer epidemiology, risk factors, classification, prognostic biomarkers, as well as possible treatment options.
Keywords: breast cancer, epidemiology, risk factors, classification, diagnosis, prognostic markers, treatment
Definition
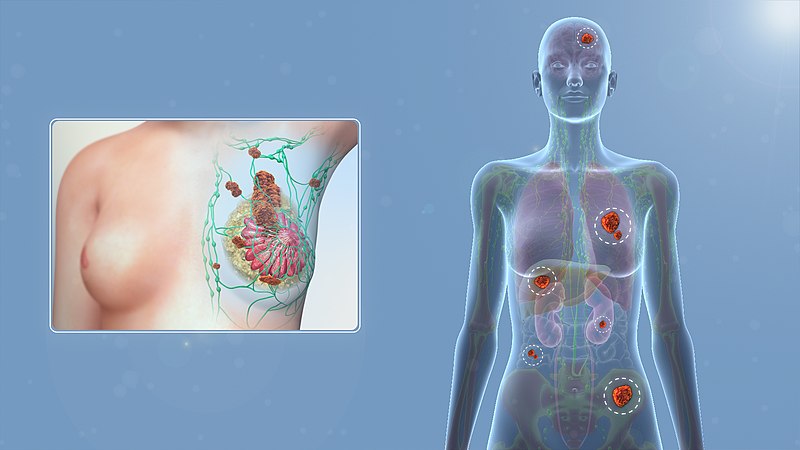
Breast cancer is an uncontrolled growth of epithelial cells originating in the ducts or breast lobules. The disorder includes early, noninvasive breast cancer, such as ductal carcinoma in situ (DCIS) or lobular carcinoma in situ (LCIS), breast cancer that has invaded the surrounding breast stroma (primary invasive breast cancer); and breast cancer that has spread to the draining lymph nodes or to distant organs (advanced or metastatic breast cancer)
Introduction
Breast cancer is the most common cancer overall among women in both developed and less developed countries of the world, and the second cause of death in developed regions after lung cancer. Despite its increasing incidence, breast cancer mortality has been decreasing in most high-income countries of Europe and North America due to screening, early detection and access to adjuvant treatments. Indeed, screening programs are estimated to have reduced breast cancer mortality by 20% in the invited population. In addition, breast cancer is one of the fields in oncology that has seen some major advances in the understanding of the underlying biology with the molecular characterization into distinct entities, as well as changes in terms of treatment and prognosis in the last 15 years
Epidemiology
Worldwide, breast cancer is one of the leading causes of cancer morbidity and mortality. According to the status report on the GLOBOCAN 2018 estimates of cancer incidence and mortality, breast cancer was the second most commonly diagnosed malignancy, accounting for more than 11.6% of all female cancers. It ranked as the fifth commonest cause of cancer deaths, leading to 6.6% of all cancer mortality worldwide. It induces a substantial public health burden, leading to a loss of 14.8 million. The incidence of breast cancer is significantly higher in developed countries; globally, its age-standardized incidence rate was 54.5 per 100,000 female population in countries with high or very high Human Development Index (HDI) as compared to 31.3 in nations with low to medium HDI.
Risk factors
Non-modifiable risk factors
- Getting older. The risk for breast cancer increases with age. Most breast cancers are diagnosed after age 50.
- Genetic mutations. Women who have inherited changes (mutations) to certain genes, such as BRCA1 and BRCA2, are at higher risk of breast and ovarian cancer.
- Reproductive history. Starting menstrual periods before age 12 and starting menopause after age 55 expose women to hormones longer, raising their risk of getting breast cancer.
- Having dense breasts. Women with dense breasts are more likely to get breast cancer.
- Personal history of breast cancer or certain non-cancerous breast diseases. Women who have had breast cancer are more likely to get breast cancer a second time
- non-cancerous breast diseases such as atypical hyperplasia or lobular carcinoma in situ are associated with a higher risk of getting breast cancer.
- Family history of breast or ovarian cancer. A woman’s risk for breast cancer is higher if she has first-degree relative or multiple family members on either her mother’s or father’s side of the family who have had breast or ovarian cancer. Having a first-degree male relative with breast cancer also raises a woman’s risk.
- Previous treatment using radiation therapy. Women who had radiation therapy to the chest or breasts (for instance, treatment of Hodgkin’s lymphoma) before age 30 have a higher risk of getting breast cancer later in life.
- Exposure to the drug diethylstilbestrol (DES). DES was given to some pregnant women in the United States between 1940 and 1971 to prevent miscarriage. Women who took DES, or whose mothers took DES while pregnant with them, have a higher risk of getting breast cancer.
Modifiable risk factors
- Not being physically active
- Being overweight or having obesity after menopause.
- Taking hormones. Some forms of hormone replacement therapy (those that include both estrogen and progesterone) taken during menopause can raise risk for breast cancer when taken for more than five years. Certain oral contraceptives also have been found to raise breast cancer risk.
- Reproductive history. Having the first pregnancy after age 30, not breastfeeding, and never having a full-term pregnancy can raise breast cancer risk.
- Drinking alcohol. Studies show that a woman’s risk for breast cancer increases with the more alcohol she drinks.
Classification
Invasive breast cancer is currently classified as non-specific ductal carcinoma and specific subtypes. Special subtypes of breast cancer have specific definitions, while the non-specific type contains all carcinomas other than specific subtypes
Microscopic Grading in Breast Carcinoma (Nottingham Modification of the Bloom-Richardson system)
Tubule formation
1.point: Tubule formation constitutes more than 75% of the tumor
2.point: Tubule formation constitutes 10–75% of the tumor,
3.point: Tubule formation constitutes less than 10% of the tumor.
Nuclear pleomorphism
1.point: Nucleus shape and size difference mild,
2.points: Nucleus shape and size difference moderate,
3.points: Nucleus shape and size difference significant.
Mitotic Count – Mitotic counting process should only be done at the periphery of the tumor and should be started from the most mitotic active areas.
A total score is obtained by scores on tubule formation, nuclear pleomorphism and mitotic count
Histological evaluation by this method is semi-quantitative, but provides very strong prediction for determining patient prognosis.The TNM system is used as a common language among treatment centers widely all over the world, to guide treatment planning, provide an effectiveness of the treatment during follow-up and predict prognosis. However, with advances in diagnosis and treatment of breast cancer, initiatives to evaluate tumor biology in detail, accumulation of new data showing that most prognostic factors are related to biological features of the tumor, and most importantly the observation of very different survival rates within tumors with the same TNM group and same histological type have led to the search for alternative solutions.
New beginning
Perou and Sorlie proposed “Molecular Classification” terminology in breast cancer for the first time with a comprehensive study showing the differences in gene expression in 2000. In this study breast cancer was divided into different sub-groups according to various gene expression: “Luminal” (often differentiated in two or three subgroups; reflecting ER, ER regulatory genes and the expression of genes expressed in normal luminal epithelial cells), “HER-2 positive “(reflecting ErbB2 / HER-2 amplification and overexpression),” basal “(reflecting ER, PR, and HER-2 negative and the expression of genes expressed in normal breast basal and / myoepitelial cells). It was shown that three main subtypes can be identified in a stable manner by only using genes related to ER and HER-2 phenotypes instead of using hundreds of intrinsic genes. These subtypes are ER− / HER2− (basal-like), HER2+(HER2-Enriched), and ER+/ HER2− (luminal A and B combined). Despite the ongoing debate on advantages of molecular subtyping methods of breast cancer over each other, basically luminal A, luminal B, HER2, basal and normal-like molecular subgroups represent different prognostic subgroups, has led to rapid acceptance of the proposed classification system into clinical practice.
Prognostic biomarkers
The main function after the diagnosis of invasive breast cancer is which patient should use chemotherapy, which patient should receive adjuvant therapy, and which should not. If the decision is for adjuvant therapy, the next challenge is to identify the most appropriate treatment or combination of treatments for a particular patient. Addressing the first challenge can be helped by prognostic biomarkers, while addressing the second challenge can be done by predictive biomarkers. Among the molecular markers related to BC, ER, PR, HER2, and the Mib1/Ki-67 proliferation index are the most significant ones and are tightly confirmed in the standard care of all primary, recurrent, and metastatic BC patients. CEA and CA-15-3 antigens are the most valuable markers of serum tumors in BC patients.
Treatment
Treatment for breast cancer depends on the subtype of cancer and how much it has spread outside of the breast to lymph nodes or to other parts of the body.
Doctors combine treatments to minimize the chances of the cancer recurrence.
These include:
- surgery to remove the breast tumour
- radiation therapy to reduce recurrence risk in the breast and surrounding tissues
- medications to kill cancer cells and prevent spread, including hormonal therapies, chemotherapy or targeted biological therapies.
Surgeries may include lumpectomy or mastectomy. Surgery may also remove lymph nodes to assess the cancer’s ability to spread.
Radiation therapy treats residual microscopic cancers left behind in the breast tissue and/or lymph nodes and minimizes the chances of cancer recurring on the chest wall.
Medical treatments for breast cancers, which may be neoadjuvant or adjuvant, is based on the biological subtyping of the cancers. Cancer that express the (ER) and/or (PR) are likely to respond to hormone therapies such as tamoxifen or aromatase inhibitors. Cancers that do not express ER or PR are “hormone receptor negative” and need to be treated with chemotherapy unless the cancer is very small.Breast cancers may independently overexpress a molecule called the HER-2/neu oncogene. These “HER-2 positive” cancers are amenable to treatment with targeted biological agents such as trastuzumab. When targeted biological therapies are given, they are combined with chemotherapy to make them effective.Radiotherapy plays a very important role in treating breast cancer. With early-stage breast cancers, radiation can prevent a mastectomy. With later stage cancers, radiotherapy can reduce cancer recurrence risk even when a mastectomy has been performed. For advanced stage of breast cancer, in some circumstances, radiation therapy may reduce the likelihood of dying of the disease
And now,homoeopathy
In the current scenario of medical sciences, homeopathy, the most popular system of therapy, is recognized as one of the components of complementary and alternative medicine across the world. Homeopathy has been considered to be safe and cost-effectiveness therapeutic modality. However, selection of appropriate medicines against a disease is cumbersome as totality of symptoms of a patient guides the process. Available data suggest that homeopathy has potency not only to treat various types of cancers but also to reduce the side effects caused by standard therapeutic modalities like chemotherapy, radiotherapy or surgery.
Homoeopathy is among the commonly used alternative approaches in Cancer. It is being widely used as palliative and curative in patients suffering from cancer. Studies on the use of Homoeopathy in cancer after surgery, radio therapy and chemotherapy have been reported. It was found that beneficial effect of Homoeopathic medicines are reported on some cancer cell lines via apoptosis and immune modulation. Homoeopathic treatment given as add on also improves the quality of life, survival time and presenting complaints. However, more evidence needs to be generated to demonstrate anti tumor or antimetastatic potential in controlled clinical trials.
About Author
Dr. Prajkta khanvilkar, MD Scholar, Batch 2020-21, Department of Practice of Medicine, Government Homoeopathic Medical College and Hospital, Bhopal, Madhya Pradesh



