Abstract:
Irritable bowel syndrome is one the gastrointestinal disorder which has correlation with the central nervous system. Biopsychosocial model of irritable syndrome plays a significant role in patient life. This article provides information regarding mind and gastro intestinal system correlation with each other. This article shows rubric anxiety shows correlation with abdomen and how homoeopathy will cure the disease condition.
Keywords:
Irritable bowel syndrome, anxiety, brain gut axis.
Introduction
IBS is characterized by the presence of abdominal pain associated with disturbed defecation. Bloating is often present, but this is not considered an essential symptom for diagnosis. Individual symptoms are neither sensitive nor specific enough on their own to diagnose IBS.
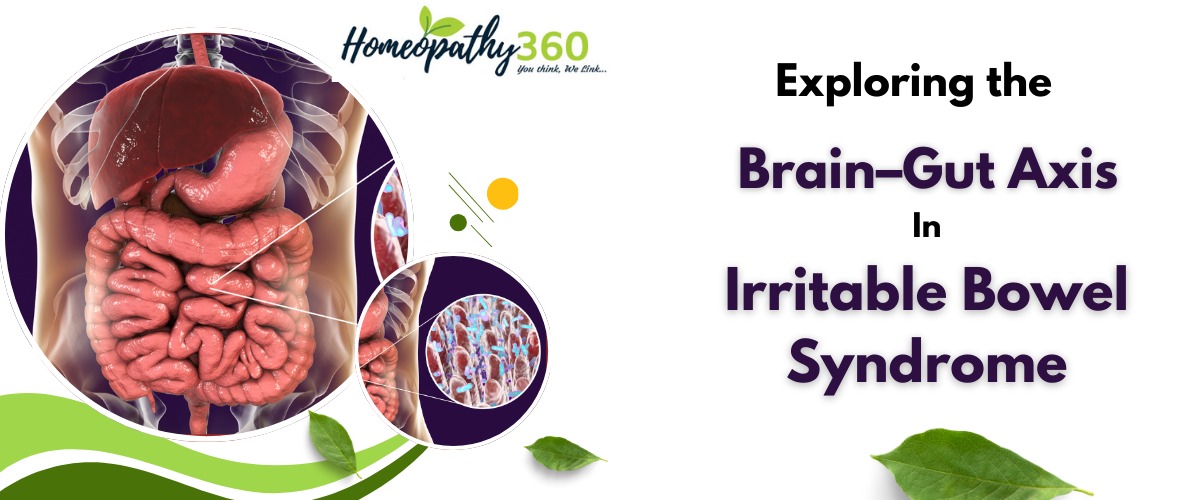
Mechanism of Brain Gut Axis
The brain-gut axis is a neuroanatomic substrate in which the psychosocial factors just described influence the GI tract and vice versa. The “hardwiring” is a complex integrated circuitry that communicates information between the CNS and myenteric plexus to the end-organ structures. It is a bidirectional system in which thoughts, feelings, and memories lead to neurotransmitter release (the software) that affects sensory, motor, endocrine, autonomic, immune, and inflammatory function. Gut microbiota also engage in bidirectional communication with the brain via neural, endocrine, and immune pathways with significant consequences for behavioral disorders including anxiety, depression, and cognitive disorders as well as chronic visceral pain. Dysregulation of this system explains motility disturbances, pain and other GI symptoms, and functional gastrointestinal disorders. In effect, the brain-gut axis is the neuroanatomic and neurophysiologic substrate for the clinical application of the biopsychosocial model.
Psychological aspect of Irritable Syndrome
Patients with IBS are more likely to report greater lifetime and daily stressful events than those with organic disease or healthy controls, and may be more susceptible to stress-altered GI function. Stress in healthy volunteers changes intestinal secretion and permeability responses. Sustained stress might, therefore, be important in both the onset and persistence of IBS. In patients with IBS, a history of sexual, physical, or emotional abuse is reported more often than in those without IBS. Abuse has not been shown to alter rectal sensation, but it might modulate central responses to pain. Psychiatric conditions including depression, anxiety, and somatization often coexist in IBS. Consultation (referral) bias may explain the higher rates of psychologic and psychiatric comorbidity seen in IBS patients compared with controls, but other data suggest the association is real. These observations have led some to consider IBS as a braingut disorder, with the brain driving the GI and noncolonic symptoms seen in sufferers. The mechanisms for this are discussed later. However, psychologic comorbidities seen in IBS, rather than being a primary problem, might occur secondary to bowel dysfunction. There is evidence to suggest that in about 50% of individuals with psychologic disorders, GI symptoms arise first, and a new-onset mood disorder develops later suggesting a gut-brain disorder in a subset of these patients. Evidence to support this implicates intestinal inflammation, the cytokine response, and the intestinal microbiome in precipitating such gut-to-brain alterations. Immune activation of the intestine with elevated TNF-α levels has been linked to anxiety and depression, and blocking TNF-α may reverse these brain changes, suggesting that mood disorders in IBS might occur secondary to intestinal inflammation in some cases.
Central Nervous System Affection
As discussed earlier, individuals who experience early adverse life events, such as trauma or abuse, are more likely to develop IBS, and mood disorders are more common among patients with IBS. This has led to the concept of IBS being a disorder of the intestine that is driven by brain abnormalities. Investigators have shown reduced inhibitory feedback on the emotional arousal network, which is important for autonomic control of GI function, and increased activity following visceral stimuli. Central processing of sensory information is aberrant in some individuals. The extent of these changes is correlated with the duration and severity of symptoms, suggesting structural brain changes in response to these stimuli. There also may be increased engagement of regions of the brain that are concerned with attentional and behavioral responses to both the arrival of, and the anticipation of, such stimuli, and heightened awareness of, or attention to them, with reduced activity in areas of the cortex that should inhibit or downregulate the response.
In another study recruiting patients with IBS in whom anxiety and depression levels were comparable to healthy controls, activity levels of the dorsolateral prefrontal cortex were impaired during behavioral selection tasks among those with IBS. This suggests that, even when there is no evidence of anxiety or depression, patients with IBS have CNS dysfunction, which may make them vulnerable to stressors. Finally, adverse events in early life can shape adult resting state connectivity in the salience/ executive control network, a brain network that has been implicated in the pathophysiology of central pain amplification.
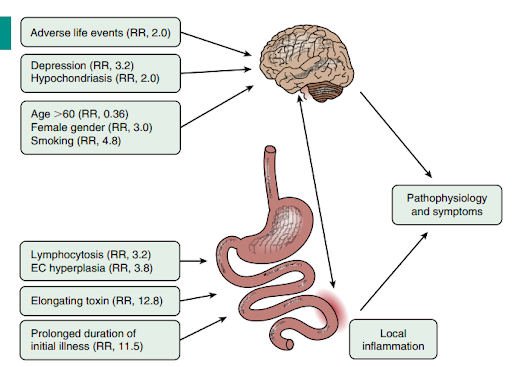
Image 1 Brain GUT axis of irritable bowel syndrome
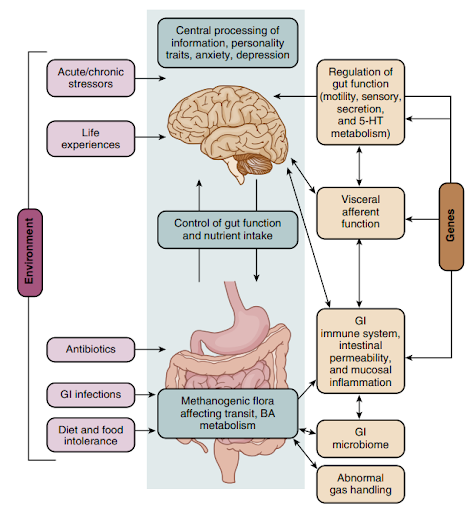
Image 2 Brain GUT axis of irritable bowel syndome
Repertorial correlation irritable bowel syndrome
- ANGUISH pain in abdomen, with (18)
2 calc, 1 cham, 1 coff, 1 colch, 2 coloc, 1 cupr, 2 cupr-ar, 2 dios, 1 ham, 1 lach, 1 merc-c, 1 merc-pr-r, 1 naja, 1 nit-ac, 1 plb, 1 sul-ac, 1 tab, 2 verat
- ANGUISH tossing about, with tearing in abdomen, with (1)
3 CHAM
- ANXIETY abdomen arising from (2)
1 asaf, 1 dig
- ANXIETY abdomen in (82)
1 acon, 1 agar, 1 aloe, 1 alum, 1 am-m, 1 ambr, 1 anac, 1 androc, 1 ant-c, 3 ANT-T, 1 apoc, 1 arg-n, 1 arn, 3 ARS, 1 ars-s-f, 2 asaf, 2 aur, 2 bar-c, 1 bell, 1 bry, 1 calc, 1 calc-p, 1 calen, 1 carb-an, 1 carb-v, 1 carl, 1 cast-eq, 1 cham, 1 colch, 1 con, 3 CUPR, 1 dig, 1 dios, 1 dros, 1 euph, 1 gran, 1 grat, 1 hydr, 1 ign, 1 inul, 2 kali-c, 1 lach, 1 laur, 1 lept, 1 lyc, 1 mag-m, 1 mag-p, 1 merc, 1 merc-c, 2 mez, 2 mosch, 1 mur-ac, 1 naja, 1 nat-m, 1 nat-p, 1 nit-ac, 1 nux-v, 1 olnd, 1 ozone, 1 petr, 1 ph-ac, 1 phel, 1 phos, 1 pic-ac, 1 plat, 1 plb, 1 podo, 1 rhod, 1 rhus-t, 1 seneg, 1 sep, 1 spig, 1 squil, 1 staph, 1 stram, 1 sul-ac, 2 sulph, 2 tarent, 1 thuj, 1 tub, 1 verat, 1 vesp
- ANXIETY abdomen in griping, as if intestines would be constricted (1)
1 spig
- ANXIETY abdomen in flatus amel. (1)
1 mur-ac
- ANXIETY abdomen in restlessness, with anxious (1)
1 alum
- ANXIETY abdomen in extending heart, to (1)
1 thuj
- ANXIETY abdomen in hypochondria (12)
1 acon, 1 anac, 2 arn, 1 cham, 1 dig, 1 dros, 1 grat, 1 naja, 2 nux-v, 1 ph-ac, 1 phos, 1 staph
- CONFUSION injury, after abdomen, to (1)
1 ant-s
- DELIRIUM abdomen, with swelling of (2)
2 acet-ac, 1 plb
- DISCONTENTED, pain, during abdomen, in (1)
1 bac
- EXCITEMENT, pain, during abdomen, in, during each paroxysm (1)
2 coloc
- RESTLESSNESS, abdomen distension in, at night (6)
1 calc-s, 1 caust, 1 chel, 1 lyc, 1 mag-c, 1 valer
- SHRIEKING, cramps in abdomen, in (7)
1 coloc, 1 cupr, 1 hyos, 2 jatr, 2 lyc, 2 mag-p, 1 plb
- THOUGHTS abdomen, as if from (1)
1 thuj
- WORK aversion to mental abdomen, coming from (1)
1 ant-t
References:
- Homoeopathic software CARA PRO version v 1.4, Complete Repertory.
- Sleisenger and Fordtran’s Gastrointestinal and Liver disease, 11th Edition.