Osteoarthritis (OA) is a prevalent degenerative joint disease that affects millions worldwide, leading to significant pain and disability. A comprehensive clinical approach to managing osteoarthritis involves not only understanding the patient’s medical history and symptoms but also employing targeted questionnaires and assessments to guide treatment. In this article, we will explore essential questions that doctors should ask to gain a clearer understanding of a patient’s condition, outline an effective questionnaire, discuss the latest treatments available, and recommend key investigations that can aid in diagnosing and managing OA. By adopting a thorough and patient-centred approach, healthcare providers can better address the challenges posed by this chronic condition, ultimately improving the quality of life for those affected.
Let’s Understand Osteoarthritis
Osteoarthritis (OA) is by far the most common form of arthritis. It shows a strong association with ageing and is a major cause of pain and disability in the elderly.OA is a degenerative joint disease that causes pain, stiffness, and swelling in the joints. Pathologically, it can be defined as a condition of synovial joints (Synovial joints are characterised by a joint cavity that contains synovial fluid, which lubricates and nourishes the joint. Synovial joints are also known as diarthroses, which means they are freely mobile.) in which there is focal loss of articular hyaline cartilage with proliferation of new bone and remodelling of joint contour. The disease manifests first as a molecular derangement (abnormal joint tissue metabolism) followed by anatomic, and/or physiologic derangements (characterized by cartilage degradation, bone remodelling, osteophyte formation, joint inflammation and loss of normal joint function), that can culminate in illness
What are the Risk Factors for the development of OA?
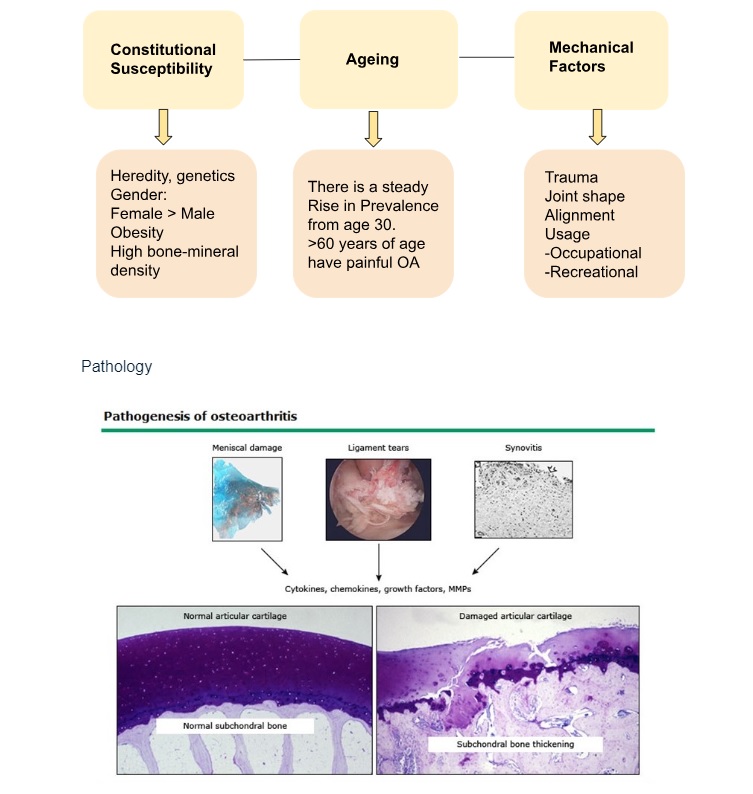
Osteoarthritis involves all of the joint tissues including the menisci in the knee, ligaments, synovium, articular cartilage, and bone. Damage to the menisci and ligament tears not only alter joint mechanics but, along with the inflamed synovium (synovitis), produce proinflammatory factors (cytokines and chemokines) and matrix-degrading enzymes (eg, matrix metalloproteinases [MMPs]). These factors are also produced by chondrocytes and serve to promote joint tissue destruction.
Questionnaire for Case Taking in Osteoarthritis:
Patient History
- Symptoms:
- What specific joints are affected?
- Can you describe the pain (e.g., sharp, dull, throbbing)?
- When did you first notice these symptoms?
- Pain Characteristics:
- How would you rate your pain on a scale from 1 to 10?
- Does the pain worsen with activity or improve with rest?
- Are there any specific movements that exacerbate the pain?
- Duration and Progression:
- How long have you been experiencing these symptoms?
- Has the pain or stiffness worsened over time?
- Morning Stiffness:
- Do you experience stiffness in the morning? If so, how long does it last?
Lifestyle and Function
- Daily Activities:
- How does the pain affect your daily activities or hobbies?
- Are there any activities you have had to stop or modify due to your condition?
- Exercise:
- Do you engage in regular exercise? If so, what type?
- How does exercise affect your symptoms?
Medical History
- Previous Treatments:
- What treatments have you tried (medications, physical therapy, etc.)?
- Have any treatments provided relief?
- Other Health Conditions:
- Do you have any other medical conditions?
- Are you currently taking any medications or supplements?
Family History
- Genetics:
- Is there a family history of osteoarthritis or other joint issues?
Emotional and Psychological Aspects
- Impact on Quality of Life:
- How do your symptoms affect your mood or mental well-being?
- Are there any coping strategies you use to deal with the pain?
These questions will help gather a comprehensive understanding of the patient’s experience with osteoarthritis, aiding in the formulation of an effective treatment plan.
Investigations
- Physical Examination: Most important trio of physical examinations of any musculoskeletal system is – LOOK, FEEL and MOVE .
- Gait Assessment:
Observe the patient’s walk to identify any abnormalities. A ‘duck walk’ can help differentiate knee pain from pain in the hip, lower back, or foot.
- Palpation:
Check for warmth, swelling and tenderness.
Palpate for Crepitus: Apply light pressure to the affected area with the fingertips to feel for a crackling, coarse or popping sensation from the affected area.
- Range of motion
Check for any restriction in motion of extremity. Flex and extend the knee as far as possible, comparing the affected knee to the other. The normal range is 0 degrees of extension to 135 degrees of flexion.
- Stability
When the knee flexed to 90°, check the stability of knee ligaments
- Inspect at rest: Look for any skin changes, swelling (osteophyte around the joint margins), wasting of muscle, attitude and deformity.
- Fluid assessment: Check for fluid in the knee by:
- Bulge sign: Gently press medial to the patella and then move your hand up. If the medial aspect bulges after lateral pressure, there is a moderate amount of fluid. If the medial aspect tenses but doesn’t bulge, there is a large amount of fluid.
- Patellar tap test: Place one hand above the patella and push fluid down into the knee. Then, use your other hand to push on the patella. If the patella bounces off the bone, there is fluid in the knee.
- 2. X-Ray- The plain X- Ray is majorly the first choice of investigation. Xray helps to assess the severity of structural change, a prior investigation before a surgery.
- PA view of pelvis is advised for the Hip OA.
- Standing AP view is advice for the assessment of tibio-femoral cartilage loss.
- Flexed skyline is advised for the Patello-femoral OA.
- 3. Radioisotope Bone Scan: For the assessment of discrete increased uptake in OA joints due to bone remodelling.
- 4. DEXA Scan: (Dual-energy X-ray absorptiometry scan),is a low-dose X-ray that helps to assess bone density and composition. It also allows the assessment of risk of bone breaking. DEXA is not recommended for pregnant women.
- 5. Arthrocentesis: Synovial fluid is aspirated from the OA knee from within a joint capsule for the investigation of any abnormality.

Exploring the Latest Research and Treatments in Osteoarthritis
Lipofilling procedure improves pain and function in finger osteoarthritis. For patients with painful finger osteoarthritis, a nonsurgical procedure called lipofilling – in which fat obtained from another part of the body is transferred into the arthritic joints – produces lasting improvements in hand function and especially pain
Use of HA injections: HA injections are given with the aim of reducing pain and improving functioning by supplementing the fluid within the knee joint.
Corticosteroid injections can relieve pain for a few weeks, but the number of injections you can receive each year is generally limited.
Nonsteroidal anti-inflammatory drugs (NSAIDs):Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), taken at the recommended doses, typically relieve osteoarthritis pain.
Regenerative therapies with stem cells: A total of 144 clinical trials investigating the therapeutic impact of stem cells on OA and on cartilage trauma have been reported to date at clinical trials gov, suggesting regenerative medicine may be a promising therapy for future OA management.
Anabolic drug: sprifermin and Anti-catabolic drugs: MMP inhibitors.
Reference
https://www.wolterskluwer.com/en/news/lipofilling-procedure-improves-pain-and-function-in-finger-osteoarthritis#:~:text=For%20patients%20with%20painful%20finger,issue%20of%20Plastic%20and%20Reconstructive
https://www.mayoclinic.org/diseases-conditions/osteoarthritis/diagnosis-treatment/drc-20351930
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7199286/
Davidson’s principle and practice of medicine 24th edition edited by Nicholas A.BoonNicki R. College BrianR.Walker