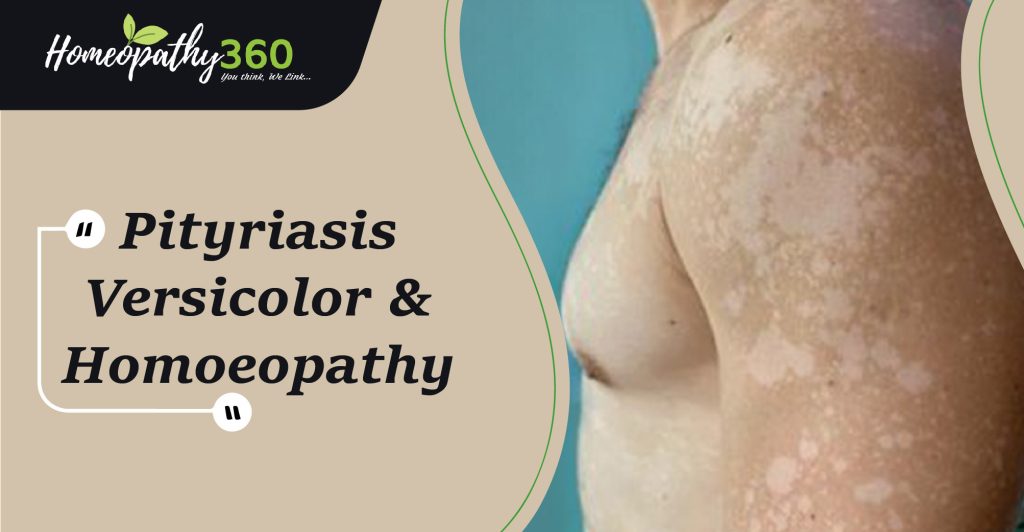
ABSTARCT– Pityriasis versicolor (PV), also known as tinea versicolor, this condition is one of the most common superficial fungal infections worldwide, particularly in tropical climates. PV is a persistent, superficial skin condition caused by various species of the commensal yeast Malassezia, most commonly Malassezia globosa, but sometimes M.sympadialis or M.furfur, It occurs in men and women and in different races. It is found more frequently in warmer, humid climates, and is usually more severe and persistent in the immunocompromised. It is characterised by scaly, oval macules on the upper trunk, usually hypopigmented [but occasionally hyperpigmented. Hypopigmentation is more obvious after sun exposure and tanning. PV is difficult to cure and the chances for relapse or recurrent infections are high due to the presence of Malassezia in the normal skin flora.
KEYWORDS – pityriasis, superficial fungal infection, Homoeopathy.
DEFINITION– Pityriasis versicolor, also known as tinea versicolor, is a frequent, superficial fungal infection of the skin. It belongs to Malassezia-related diseases. Clinical features of pityriasis versicolor include either hyperpigmented or hypopigmented finely scaly macules. The term pityriasis is used to describe skin conditions in which the scale appears similar to bran. The multiple colors of pityriasis versicolor give rise to the second part of the name, versicolor. Pityriasis versicolor is sometimes called tinea versicolor, although the term tinea should strictly be used for dermatophyte fungus infections.
The areas most often affected by pityriasis versicolor include the:
- Back
- Chest
- Upper arms
- Neck
- Proximal extremities
Epidemiology- Pityriasis versicolor has been reported worldwide, but it is more common in warm and humid conditions. The prevalence is as high as 50% in tropical countries and as low as 1.1% in cold climates such as Sweden. Pityriasis versicolor occurs more frequently in adolescents and young adults probably due to the increase of sebum production by the sebaceous glands which allow for a more lipid-rich environment in which Malassezia can grow. Pityriasis versicolor affects men and women equally and no specific ethnic predominance has been noted.
Causes- Tinea versicolor is caused by infection with the fungus Malassezia species (globosa, sympodialis, and furfur). This organism is frequently present in its yeast form as a colonizer of normal skin. In tinea versicolor, the spores proliferate in the outer layers of the stratum corneum, often beginning in the areas of follicular openings. When the spore forms are transformed to hyphae, infection occurs as the hyphal structures invade more deeply into the stratum corneum, but they do not penetrate the viable epidermis. They cause thickening and disruption of the stratum corneum. Most cases of tinea versicolor occur in healthy individuals with no immunologic deficiencies. Nevertheless, several factors predispose some people to develop this condition. These factors include genetic predisposition; warm, humid environments; immunosuppression; malnutrition; application of oily preparations; corticosteroid usage; and Cushing disease. The use of bath oils and skin lubricants may increase the risk of developing tinea versicolor.
Clinical features-
- A person is likely to notice tinea versicolor only when spots start to appear on the skin. These spots may be lighter or darker than the surrounding skin, and are often more noticeable when the surrounding skin is tan.
- Though most common around the trunk and neck, these spots may appear anywhere on the body.
- Itchy patches of spots
- Spots that grow slowly over time, potentially forming into patches
- Symptoms may disappear or become reduced in cooler weather and may return when the weather becomes hot and humid.
- Clinical findings: red scratchy scabs over back, nape of neck.
- Patients with pityriasis versicolor present with multiple, well-demarcated, oval, finely scaling patches or plaques.
- Skin lesions may be hypopigmented, hyperpigmented, or erythematous and occasionally become confluent and widespread.
- Patches of skin may be darker or lighter than your normal skin colour.
- Patches can also be red, brown or pink.
Diagnosis-Pityriasis versicolor can be clinically diagnosed by its characteristic skin lesions (erythematous, hyperpigmented or hypopigmented, finely scaling, thin plaques).The fine scale on the affected skin is not easily seen but becomes more apparent when the skin is stretched or scraped (the “evoked scale sign”). This sign is helpful in confirming a diagnosis of pityriasis versicolor. Microscopic confirmation is helpful when there is uncertainty about the diagnosis. It is not useful diagnostically after the patient is treated since it will be negative in most cases. Pretreatment diagnosis can be confirmed by microscopic examination of skin scrapings treated with potassium hydroxide or stained with Swartz Lamkin or chlorazol black. Using stains allows for easier identification of fungal forms and can be helpful for clinicians who infrequently examine slides. Alternatively, scrapings can be sent to a laboratory with a request for fungal microscopy.Examination of prepared slides reveals numerous spores and hyphae that resemble “spaghetti and meatballs.
Differential diagnosis-
Pityriasis versicolor may be confused with various conditions:
• Pityriasis rosea
• Tinea corporis
• Vitiligo
• Pityriasis alba
• Post inflammatory hypo- and hyperpigmentation
• Seborrheic dermatitis
• Guttate psoriasis
• Nummular eczema
• Secondary syphilis
• Mycosis fungoides
PREVENTION
- The most effective method of prevention is hygiene. Removing excess oils and dirt from the skin can help protect someone from contracting this infection.
- Antifungal lotions and shampoos that are available over the counter offer a good means of prevention. These same products can also help keep a mild infection under control.
- Additionally, taking some extra steps to keep dry in hot and humid weather and avoiding excessive exposure to sunlight may help to stop the growth of tinea versicolor.
Do’s in Tinea Versicolor
If you are going through Homeopathic Treatment for Tinea Versicolor, then you can do these things along with the medication that can help in this problem.
- Maintain hygiene.
- Bath daily.
- Wear cotton clothes.
- Wear loose clothes.
- Keep skin clean.
- Apply sunscreen if you are going out.
Don’ts Do In Tinea Versicolor
If you are using Homeopathic medicines for the treatment of tinea versicolor, then do not prefer these things along with the medication that can help in this problem.
- Don’t wear synthetic clothes.
- Don’t wear tight clothes.
- Don’t use harsh soaps.
- Don’t overexpose yourself to the sun
Homoeopathy Approach for Pityriasis Versicolor
Homeopathy aims to address the underlying factors that contribute to conditions like pityriasis versicolor, such as imbalances in the body’s internal environment. Homeopathic remedies are selected based on individual symptoms, overall health, and constitutional factors. The holistic approach of homeopathy can help in managing symptoms, preventing recurrence, and improving overall skin health.
Following are the few homeopathic medicines used in PV:-
- SULPHER
- PSORINUM
- BACILLINUM
- NATRUM MURITICUM
- TELLURIUM
- SEPIA
- ARSENIC ALBUM
- MEZEREUM
- GRAPHITES
- KALI SULPH
- THUJA
References
- Karray M, McKinney WP. Tinea Versicolor. StatPearls Publishing; 2022.
- Gupta AK, Bluhm R, Summerbell R. Pityriasis versicolor. J Eur Acad Dermatol Venereol [Internet]. 2002 [cited 2024 Feb 12];16. Available from: https://dermnetnz.org/topics/pityriasis-versicolor
- Pityriasis versicolor [Internet]. Dermnetnz.org. [cited 2024 Feb 12]. Available from: https://dermnetnz.org/topics/pityriasis-versicolor
- Fletcher J. Tinea versicolor: Symptoms, causes, and treatment [Internet]. Medicalnewstoday.com. 2017 [cited 2024 Feb 12]. Available from: https://www.medicalnewstoday.com/articles/315779
- Pityriasis versicolor [Internet]. HSE.ie. [cited 2024 Feb 12]. Available from: https://www2.hse.ie/conditions/pityriasis-versicolor/
- Penman ID, Ralston SH, Strachan MWJ, Hobson R, editors. Davidson’s principles and practice of medicine. 24th ed. London, England: Elsevier Health Sciences; 2022.
- Łabędź N, Navarrete-Dechent C, Kubisiak-Rzepczyk H, Bowszyc-Dmochowska M, Pogorzelska-Antkowiak A, Pietkiewicz P. Pityriasis versicolor—A narrative review on the diagnosis and management. Life (Basel) [Internet]. 2023 [cited 2024 Feb 12];13(10):2097. Available from: https://www.mdpi.com/2075-1729/13/10/2097
- Tinea versicolor: Causes, symptoms, risk factors, diagnosis, treatment and prevention [Internet]. prepladder. [cited 2024 Feb 12]. Available from: https://www.prepladder.com/neet-pg-study-material/dermatology-and-venereology/tinea-versicolor-causes-symptoms-risk-factors-diagnosis-treatment-and-prevention
- Singh J. Best homeopathic treatment for Tinea versicolor problem [Internet]. Lybrate. 2019 [cited 2024 Feb 12]. Available from: https://www.lybrate.com/topic/homeopathic-treatment-of-tinea-versicolor/7eeacbe36cbf4c4735b51d410a226266
About the Author:
Dr. Hemant Masar (MD Scholar)
Dept. Of Practice of Medicine – Govt. Homoeopathic Medical College & Hospital Bhopal
Guided By –
Dr. Bharat Singh Poosam M.D. (Hom)
Assist. Professor – Govt.Homoeopathic Medical College & Hospital Bhopal